Understanding Adolescent Idiopathic Scoliosis Correction
Recognizing the Complexity of Adolescent Idiopathic Scoliosis
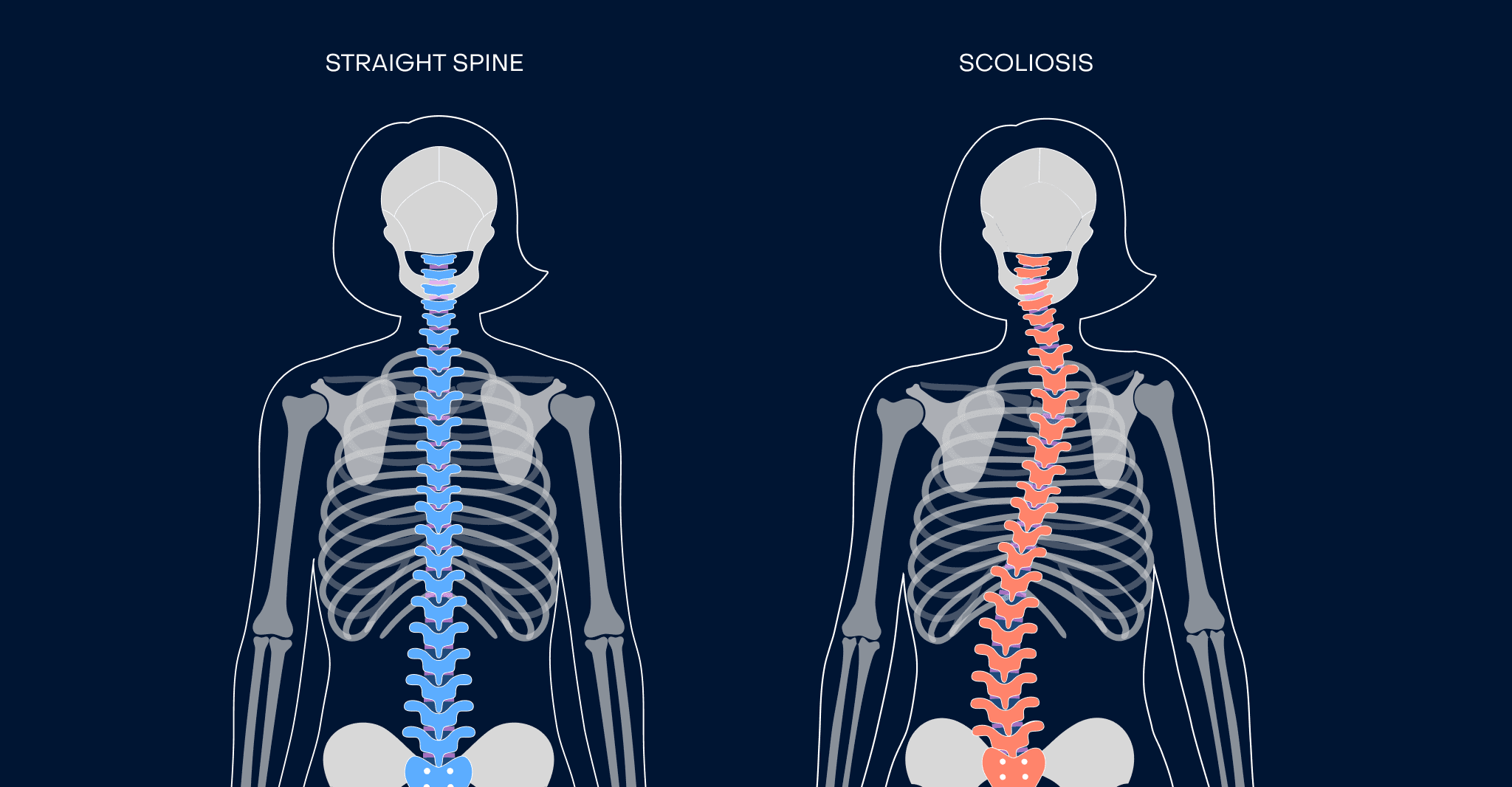
Adolescent idiopathic scoliosis (AIS) describes a condition in which the spine develops an abnormal lateral curve—typically forming an “S” or “C” shape—during growth without a known cause. “Idiopathic” itself means there is no identifiable origin, and this form of scoliosis makes up nearly 80% of all cases. It most commonly emerges between the ages of 10 and 18, striking during one of the body’s most rapid periods of growth.
For parents and adolescents, the diagnosis often brings more uncertainty than clarity. They are presented with a radiographic image of a curved spine, a Cobb angle measurement, and questions with no quick answers. Many families wonder if their child’s curve will worsen, if it will affect sports participation, or whether the changes in posture or gait signal a coming impairment. Determining whether to monitor, brace, or prepare for surgery is complex and deeply individualized.
Part of the challenge lies in how scoliosis behaves during growth spurts. A child who appears fine at age 11 may demonstrate significant progression by age 13. The curve may remain flexible or begin to stiffen. Concerns mount over potential long-term effects on back pain, lung capacity, joint health, and body image. These are not just cosmetic issues—they relate to structural bone development and spinal alignment that will influence adult life.
Engaging a scoliosis specialist early creates clarity. Dr. Firas Husban’s practice centers on understanding each adolescent’s skeletal maturity, curve behavior, and activity level—not just their x-rays. Early specialist input is often the difference between proactive care and rushed surgery decisions later. A comprehensive evaluation helps put a roadmap in place: one that balances time, risk, growth, and real quality of life.
Scoliosis Correction: When Observation Isn’t Enough
In many adolescents diagnosed with scoliosis, the initial approach is not immediate intervention but close observation. Small spinal curves—typically under 20 degrees—don’t always require active treatment. With regular imaging and clinical exams, doctors monitor curve progression during growth. This system of watchful waiting is especially effective when the spine is still flexible, and the child hasn’t reached their peak growth spurt.
The key tool in deciding treatment routes is the Cobb angle—a measurement that quantifies the degree of spinal curvature. A curve under 25° that isn’t worsening may only need observation. Between 25–40°, bracing is often recommended if growth is ongoing. However, once the Cobb angle reaches 45–50°, or if bracing fails to halt progression, surgical scoliosis correction becomes the primary recommendation.
This decision isn’t only about aesthetics. Moderate to severe spinal curves may strain the body’s biomechanics, affecting motion, flexibility, and joint wear long before adulthood. Over time, distorted spinal shape can lead to chronic back pain, limited lung function, and noticeable shoulder asymmetry. Scoliosis correction surgery aims to straighten and hold the spine in a healthier alignment, protecting both form and function in the decades ahead.
Surgical Correction: Current Options for Adolescents (Purpose, Not Procedure)
Choosing surgical correction for adolescent idiopathic scoliosis depends on multiple factors: the curve’s severity, the patient’s skeletal maturity, and the impact on their daily function. In adolescents, fusion surgery remains the central method for achieving long-term spinal stability and realignment. However, several approaches have evolved, each offering different benefits depending on the patient’s specific anatomy and needs.
The traditional method—posterior spinal fusion—uses rods, screws, and bone grafts to hold the spine in a corrected shape while the vertebrae fuse into a solid single unit. This surgery is effective for large or rapidly progressing curves, and it significantly reduces the risk of further deformity. Though recovery lasts several months, the outcomes in properly selected adolescents are both functionally and visually impressive. The fused section does not move, but patients usually retain flexibility above and below the fusion zone—preserving normal activities, including most sports.
Some adolescents, particularly those with curves between 40–60°, may be candidates for minimally invasive scoliosis surgery. This approach utilizes smaller incisions and causes less muscle trauma, which can translate to reduced blood loss, less postoperative pain, and faster recovery. However, it may not be suitable for patients with rigid curves, very large Cobb angles, or vertebral rotation—precisely the situations that make fusion necessary. The spinal structure must be flexible enough and the access paths safe enough for the technique to succeed.
Hybrid procedures and anterior approaches (such as vertebral body tethering, or VBT) may be considered in skeletally immature patients whose spine is still growing. These methods attempt to modulate growth while preserving spinal motion, but they remain reserved for select cases due to variable long-term outcomes and a higher rate of reoperation.
Dr. Firas Husban’s evaluation process is tailored: he assesses not only the structural shape of the spinal curve but also the patient’s age, skeletal maturity, flexibility, and goals. For instance, a 16-year-old gymnast with a 52° thoracolumbar curve may benefit more from a traditional posterior fusion due to the curve’s rigidity and her nearing end of growth. In contrast, a 12-year-old boy with a 43° curve and significant spine flexibility might be considered for a less invasive option if feasible. Below is a simplified comparison of surgical approaches available:
- Posterior Spinal Fusion: Most common; excellent long-term correction; some flexibility lost; recovery time moderate to long.
- Minimally Invasive Fusion: Less postoperative pain; shorter hospital stay; applicable in select flexible curves with less deformity.
- Anterior Options (e.g., VBT): Preserves motion; ideal for younger teens still growing; long-term durability still under study.
Ultimately, no single solution fits all. The decision requires matching the curve’s mechanical behavior with the adolescent’s biological development—and aligning that with their physical goals and social context. That’s the framework Dr. Firas Husban applies to every scoliosis surgery evaluation.
What Sets Adolescent Correction Apart from Adult Scoliosis Surgery
While both teens and adults may require scoliosis surgery, the goals, mechanisms, and risks differ significantly. Adolescents typically experience idiopathic curves without associated health conditions. Their vertebral bones are still maturing, and spinal flexibility remains high, which makes surgical realignment more achievable. As a result, adolescents often benefit from more complete curve correction and retain better spinal motion after surgery.
In contrast, adults tend to develop scoliosis as a result of spinal degeneration—often involving disc collapse, vertebral remodeling, and joint pain. Their curves are generally less flexible and more painful, and surgeries focus more on pain relief and functional improvement than full correction. Fusion levels may be longer and involve stabilizing the lower spine and pelvis. Recovery is often slower, and complications more likely due to age-related risk factors and other medical conditions.
These differences underscore the importance of choosing a surgeon experienced in both adolescent and adult scoliosis. A dual-specialized provider like Dr. Husban understands how early treatment in teens can prevent the need for complex surgeries later in life—and how to tailor interventions precisely to a patient’s growth stage and spine health.
Questions to Ask Before Choosing Scoliosis Correction Surgery
Parents and teens preparing for scoliosis surgery often feel overwhelmed—but the right questions can clarify choices and restore a sense of control. A thoughtful surgical consultation should never feel rushed or limited to a quick decision. Instead, it’s a dialogue that defines what the surgery aims to achieve and how to plan for success.
- What is the long-term goal? Will the surgery seek to straighten the curve entirely, stop it from progressing, or both? Will it help preserve spinal flexibility where possible?
- What risks are specific to my child? Every case is different. Ask about infection risk, the potential for nerve complications, blood loss, or future bowing near the fusion segment.
- How will recovery be managed? Is there a pain protocol? When can your child return to school, sports, or physical therapy? Will spinal braces be needed after surgery?
- Who will be part of the care team? Will you meet with a nurse coordinator, physical therapist, or anesthesiologist before surgery? Is there a point person after discharge?
- What is the surgeon’s experience? How many adolescent corrections has the specialist performed in the past year? What were their outcomes?
Dr. Firas Husban’s consultations are structured step-by-step. He reviews current and past imaging to check curve progression, compares them to growth stage markers, and walks families through the thoracic and lumbar anatomy represented. Questions are encouraged. Teens are invited to express their lifestyle goals: sports, body image, future concerns. Families leave with realistic expectations and a documented plan—whether it’s observation, bracing, or surgical preparation. Having access to his support team means follow-up questions can be addressed quickly and with full context in mind.
Role of Non-Surgical Scoliosis Management
Not every adolescent with scoliosis requires surgery. In many cases—particularly when the spinal curve is moderate, flexible, and detected early—non-surgical management strategies can yield meaningful results. These approaches may not permanently reverse the curvature but can stabilize it, relieve symptoms, and help avoid or delay surgery.
Bracing remains a cornerstone of non-surgical scoliosis care, especially during periods of active growth. When used correctly, a brace can reduce curve progression in adolescents with curves ranging from 25–40 degrees. However, bracing effectiveness depends on consistent wear (18–23 hours per day for most types), curve type, and compliance. It doesn’t straighten the spine but can slow or stop the progression if initiated before skeletal maturity.
Physical therapy, particularly the Schroth method, is another support modality. This specialized exercise system helps improve strength, posture control, and breathing by targeting the asymmetries caused by the spinal curve. While evidence is still emerging, in motivated patients it may help enhance bracing effectiveness or support long-term spinal health in lower-risk cases. Motion-focused approaches provide a way to manage pain if present and increase self-awareness of the body’s alignment.
Importantly, non-surgical options should never substitute for appropriate surgical advice when the curve becomes severe or shows rapid progression. Delaying surgery without guidance might lead to worsened deformity, stiffer curves, and reduced surgical outcomes. Dr. Firas Husban emphasizes that non-surgical management must be personalized—aligned with the curvature’s behavior and the patient’s growth status. If non-surgical methods offer real benefit, he supports them fully. If they only serve to postpone an inevitable surgery, he explains that clearly and compassionately, allowing families to make fully informed decisions.
The Experience with Dr. Firas Husban: A Specialist’s Approach
Choosing where and how to pursue scoliosis correction is as important as choosing whether to treat at all. Dr. Firas Husban brings a unique perspective: a combination of neurosurgical and orthopedic expertise, focused specifically on spinal deformity. His background allows him to evaluate idiopathic scoliosis not just as a matter of spinal alignment but as a biomechanical and neurological system that affects a patient’s entire function and health trajectory.
Dr. Husban treats both adolescents and adults, and that dual experience informs his planning. For adolescent patients, he evaluates growth potential, lifestyle goals, curve location, and spinal flexibility before recommending any intervention. His team works collaboratively—combining radiologic analysis, surgical modeling, and patient lifestyle interviewing to create a treatment plan that’s both medically sound and personally meaningful.
The process begins with a comprehensive spine evaluation, including EOS low-dose imaging if appropriate, and side-bending x-rays to assess flexibility. These tests help determine whether a curve is likely to progress or respond to correction. The adolescent’s maturity stage—measured by markers like Risser sign or menarche in females—is factored into treatment timing. This biological perspective ensures that bracing isn’t attempted too late and that surgery isn’t performed prematurely.
Dr. Husban employs minimally invasive scoliosis correction when the patient’s spinal curve and anatomy support it but never compromises correction goals for cosmetic outcomes alone. If open posterior spinal fusion is needed, he explains each phase—how rods and screws support the spine, how vertebrae fuse over months, and what the fusion means for future motion and activity. He encourages pre-operative physical conditioning when suitable and ensures that post-operative care includes pain management, walking protocols, and monitored return to activity.
Example Case: A 15-year-old athletic girl presented with a 48° thoracic curve. She had tried bracing for over a year with increasing discomfort and visible deformity. Her COBB angle progressed steadily, and her curve showed signs of rotation and stiffness. After reviewing imaging and discussing sports goals and concerns about appearance, the family chose spinal fusion. Surgery was performed using a posterior approach, correcting curvature to 14°, with full return to non-impact sports by month six. The patient felt more comfortable in her appearance and reported improved posture and breathing—a major improvement in both function and confidence.
Dr. Firas Husban’s approach prioritizes respect, clarity, and individualized outcomes. Patients and families are guided not toward a default option, but toward a plan rooted in anatomy, growth, and whole-body wellness.
How to Prepare for a Scoliosis Evaluation
Attending a scoliosis evaluation can transform anxiety into understanding, especially when patients come prepared. Bringing relevant imaging is crucial. If an MRI, x-ray, or CT scan was previously performed, it should be included even if it’s older. A key piece of information to share during the visit is growth history: changes in height, milestones such as the onset of menstruation in girls, and any recent growth spurts often indicate how much growth remains.
Families are encouraged to prepare key questions from earlier sections—especially about surgical goals, recovery support, and the specifics of bracing history if applicable. It also helps to write down any symptoms the adolescent has experienced, such as back pain, fatigue with sports, breathing difficulty, or changes in body shape—these often go unnoticed during a standard physical exam.
Meeting with a scoliosis specialist like Dr. Firas Husban is not a commitment to surgery. It is a chance to better understand the shape, behavior, and risks of a spinal curve with expert input. Whether the outcome is continued monitoring, bracing, or planning a correction, the evaluation provides a clearer map forward—for both patient and family.
Conclusion: Confident Decisions Through Expert Guidance
Adolescent idiopathic scoliosis can be a highly individual and unpredictable condition—one where outcomes depend heavily on timely, tailored decisions. A spine that bends during a growth surge does not always demand correction, but it never deserves dismissal. Whether the path ahead involves observation, bracing, or scoliosis correction surgery, understanding your child’s spinal health in precise terms is a gift—for their present confidence and future stability.
Scoliosis correction is not simply about undoing curvature. It’s about preserving function, preventing long-term spinal complications, and supporting adolescents as they grow—not just in height, but in life. From minimally invasive options to definitive spinal fusion, every treatment choice must account for the spine’s shape, the body’s growth, the person’s mobility needs, and the years ahead.
Dr. Firas Husban’s practice embodies this philosophy. Through a multidisciplinary lens, he evaluates the mechanical, medical, and emotional dimensions of spine correction. Teen patients and their families receive honest guidance, comprehensive resources, and compassionate care that makes complex decisions feel navigable and personalized.
If you’re navigating a new scoliosis diagnosis or preparing to revisit one that’s progressed, a comprehensive consultation with a dedicated scoliosis specialist can shift the conversation from stress to understanding—and from uncertainty to action. The spine may be curved, but the path to clarity doesn’t have to be.
Additional Resources and Next Steps
To support your understanding and planning around adolescent idiopathic scoliosis, explore the following resources available through our practice:
- Spine Specialist Consultations – Learn how Dr. Firas Husban tailors evaluations for scoliosis at every stage.
- Scoliosis Surgery Options – Compare the benefits, risks, and recovery plans for different surgical interventions.
- Minimally Invasive Spine Surgery: What to Expect – Understand when this approach may be right for an adolescent case.
- Scoliosis in Adults vs. Adolescents – Different Curves, Different Care – Explore the key distinctions in planning and outcomes.
Book a Consultation: If you’re ready to move from research to real answers, you can schedule a scoliosis evaluation with Dr. Firas Husban. Consultations are available by request through our contact page, and all records can be reviewed securely under our privacy policy. Whether you’re at the beginning of your journey or choosing among options, we’re here to support confident, informed decisions for every patient and every curve.
Post Tags :
- adolescent idiopathic scoliosis correction
- adult scoliosis correction
- best scoliosis correction surgeon in Jordan
- best scoliosis surgeon near me
- Dr. Firas Husban scoliosis correction expert
- how scoliosis correction works
- minimally invasive scoliosis surgery
- non-surgical scoliosis management
- risks and benefits of scoliosis surgery
- scoliosis braces and treatment options
- scoliosis correction
- scoliosis correction Amman
- scoliosis correction Dr. Firas Husban
- scoliosis correction for teenagers
- scoliosis correction recovery time
- scoliosis specialist
- scoliosis surgery
- scoliosis treatment
- scoliosis treatment Jordan
- spinal curve correction
- spine deformity specialist
- spine surgeon in Amman
- when do you need scoliosis surgery